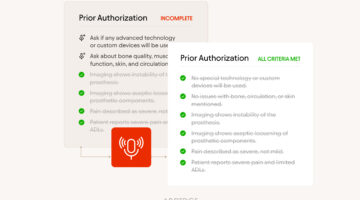
Payers Made a Bold Prior Auth Commitment in 2025. Here’s What to Expect in 2026
More than 50 major insurers have pledged to streamline prior authorization starting in 2026, but providers remain cautiously optimistic and skeptical that the changes will truly reduce burden or delays in care.